‘Hear no evil, see no evil, speak no evil’: Former Attorney-General in Victoria, Australia, on how assisted suicide legislation really works
The Honourable Robert Clark is a former Attorney-General in Victoria, Australia. He has deep knowledge of the Victorian government’s Voluntary Assisted Dying legislation and its effects. In this interview he discusses the effects of that legislation in Victoria and his views of what Kim Leadbeater’s Terminally Ill Adults (End of Life) Bill may mean for The post ‘Hear no evil, see no evil, speak no evil’: Former Attorney-General in Victoria, Australia, on how assisted suicide legislation really works appeared first on Catholic Herald.

The Honourable Robert Clark is a former Attorney-General in Victoria, Australia. He has deep knowledge of the Victorian government’s Voluntary Assisted Dying legislation and its effects. In this interview he discusses the effects of that legislation in Victoria and his views of what Kim Leadbeater’s Terminally Ill Adults (End of Life) Bill may mean for England and Wales. His comments reveal that the claim made this week in The Economist that the “takeaway from Victoria’s regime, after five-and-a-half years in operation, is that a law that looks an awful lot like Ms Leadbeater’s bill can be implemented safely” is far from the reality.
Victorian legislation on “assisted dying” is sometimes held up as a model for legislation in the UK. What is your impression of how the Victorian law is functioning?
The Victorian legislation would be a terrible model for the UK to follow. Its oversight and accountability structure seems designed on the principle of “hear no evil, see no evil, speak no evil”. In other words, designed for the regulator to find out nothing, investigate nothing and report nothing that could suggest that assisted dying has been anything other than an unblemished success. All approvals for assisted dying are given on the submitted paperwork alone, with no audits of actual compliance, no adverse event reporting requirements and no rights for concerned parties to contest.
Even with its limited accountability, some consequences of the Victorian regime have already become clear.
Firstly, the numbers of cases of assisted dying have been far higher than advocates predicted, and case numbers are continuing to grow.
Secondly, the provision of assisted dying has been concentrated with a small number of practitioners. For example, the Voluntary Assisted Dying Review Board reported that in 2023-24 the ten doctors with the highest VAD case load co-ordinated or consulted on 55 per cent of all VAD cases. This means that large numbers of patients are being counselled by doctors who have a strong personal commitment to assisted suicide.
Thirdly, VAD has been institutionalised throughout the Victorian hospital system, to the point that many doctors involved in end-of-life care who have concerns about VAD feel unable to express those concerns due to fear of adverse professional or career consequences if they do so, or are leaving the hospital system altogether.
Fourthly, the regulatory focus has been on ensuring the paperwork on the regulatory body’s files is in order, rather than on whether the legislation actually has been complied with.
What data is available and what data is missing?
The data that are published in Victoria are a bland range of the numbers of cases that have progressed through the various stages through to death, some demographic data and data on practitioner involvement. There is also some data on palliative care receipt, but nothing to indicate whether such palliative care receipt means the patient is simply on the books of a palliative care service, or whether they are actually receiving the level of care they need.
Important statistical data not reported on by the Board include the reasons for patients seeking VAD, not just their underlying medical conditions, the specialities of the doctors actually handling VAD cases, and the times that elapse between approvals for VAD and the patients’ deaths.
Crucially missing as well is any detail on the reasons why some applications for permits for VAD were not granted or what investigations, if any, the Review Board undertook of those cases. Also concerning is that there were nil applications not granted within the last two years. Rather than this being due to 100 percent practitioner compliance with the legislation, the Review Board’s latest annual report makes clear this has been achieved by the expedient of applications not being formally determined until the initially submitted paperwork has been gotten into order. The public is given no idea of how defective initially submitted paperwork has been, let alone how defective actual compliance has been.
Has there been any effect on general suicide?
There is no evidence of a reduction in general suicide in Victoria compared with other Australian states since the commencement of the VAD regime, and indeed there is some evidence of an increase in suicides amongst those aged 65 and over. This is in stark contrast to the repeated claims of advocates at the time that the legislation would help avoid suicides by people with terminal illnesses.
Indeed, even the evidence on which those claims were based – evidence produced by the Victorian Coroners Court from their statistical database – was later heavily qualified by the Coroners Court itself, pointing to limitations in its data coding and analysis and observing that grouping the data in the way the Court had initially presented might not ultimately be a useful exercise.
Are the palliative care needs of terminally ill people being met?
Victoria has serious ongoing shortfalls in palliative care, especially high-level specialist palliative care, and particularly in rural and regional areas. At the time the VAD legislation was passed in 2017, palliative care services estimated that 10,000 patients a year were dying in avoidable pain due to the absence of palliative care, compared to the 150 or so patients a year who advocates estimated would want VAD. Many of the examples of painful and distressing deaths raised in the Parliamentary debate were examples that palliative care experts pointed out could have been readily avoided with proper palliative care and if the treating doctor had the professional knowledge they should have had to refer their patient to a suitable palliative care practitioner.
Since VAD was legalised, while there have been some announcements of increases in palliative care funding, announcements such as these often simply go towards meeting increasing needs or covering increased costs, without actually improving availability levels.
The government and health bureaucracy have given far greater priority to achieving the universal availability of assisted suicide than the universal availability of palliative care. For example, they have introduced a statewide lethal substance delivery service but not a statewide pain relief medication delivery service, even though many patients in need of pain relief live in remote parts of the state. Widespread shortfalls in the availability of palliative care, particularly high-level palliative care, place patients at risk of deciding to accept assisted suicide as a very poor second choice when they would not have done so if they could have obtained the palliative care they needed.
What part is fear or existential angst playing in patients’ take-up of assisted dying?
One of the failings of the Victorian VAD regime is that the Review Board doesn’t publish data on the reasons for patients seeking VAD. However, from what practitioners have said, existential fear and distress about what may lie ahead – often unfounded – rather than physical pain or distress is a major factor in patients seeking VAD in Victoria. This is consistent with experience in other jurisdictions.
How is the legislation impacting doctors on the ground? Who does, and who does not, get involved? What is the impact on relatives and wider society?
The legislation in Victoria has had a major impact on doctors whose practice involves end-of-life care, whether in hospitals or in the community.
The government and the central health bureaucracy have pushed all public hospitals that may have terminally ill patients to make VAD readily available to the point where, as mentioned earlier, many practitioners working in public hospitals now feel unable to raise concerns lest they suffer adverse professional or career consequences.
As also mentioned earlier, outside of hospitals, there has been a high concentration of the provision of VAD with a small number of doctors, many of whom have been long term supporters of and advocates for VAD legalisation, and who have geared their practices to process the paperwork involved. This has created a serious risk that doctors holding such views will be so predisposed to regard VAD as the best outcome that they will be blind to what palliative care would be able to do for their patients, and blind to the risks that a patient seeking VAD may be lacking legal capacity, suffering from treatable depression or subject to subtle coercion or undue influence from family or friends. Indeed, there is a further risk that some doctors will push the law even beyond breaking point in order to give their patients what they regard as the benefit of assisted suicide.
It’s clear that the legalisation of VAD in Victoria and other states has meant VAD is a topic now frequently raised with doctors by terminally ill patients and their families. While some may figure it is a good thing that people know they have that choice, it creates the risk that family and friends will unconsciously see VAD as a way of resolving their own distress and feelings of helplessness in the face of the patient’s distress, rather than pushing to get better care for the patient. It also creates scope for subtle steering of a patient’s views by offspring who are quietly counting the days until they can get their hands on their inheritance. Needless to say, elder abuse is as serious a problem in Victoria as it is elsewhere, and terminally ill patients dependent on their adult children for care are particularly vulnerable.
Do you have any comments on Kim Leadbeater’s Terminally Ill Adults (End of Life) bill?
Based on the Victorian experience, heading my list of concerns about the Leadbeater Bill are two concerns in particular – firstly, the inevitable and systemic adverse effects for patients that any assisted suicide regime will create, and secondly, how the Bill’s High Court provisions will operate.
To me, the single worst effect of bringing assisted suicide into a health system is that it will change medical practice in ways that result in many patients accepting assisted suicide because they haven’t been properly informed about and reassured that fears they hold are in fact unfounded.
In other words, assisted suicide will often not be a matter of informed and considered patient choice, it will be due to assisted suicide creating systemic tendencies within the health system that lead to outcomes for many patients based on deficient advice from service providers.
This result is inherent in the nature of a medically assisted suicide regime and won’t be overcome by any claimed safeguards, however extensive.
A health system, like many other service sectors, is one where there is a huge imbalance of knowledge and power between consumer and service provider, and thus where the consumer is highly dependent on the advice and recommendations of the service provider.
With all such sectors, there is a heavy obligation on the regulator, in this case, Parliament, to ensure that the legal framework within which the sector operates does not expose consumers to systemic risks.
The imbalance of knowledge and experience between doctor and patient means the patient is dependent on the treating doctor, not only for facts, but for explicit or implicit recommendations, and for emotional reassurance. Thus, for many patients, it will be how their conversation goes with their treating doctor that determines whether they decide to go with assisted suicide or decide to go with palliative care.
On the one hand, a patient may conclude along the lines:
“I don’t want to die, but I don’t know if I can go through with what is going to happen from here. Doctor says they will do their best to relieve my pain, but she can’t guarantee the results. I asked about assisted dying, and doctor says that at this stage many patients choose that as an option and it’s something I should seriously consider. I think that’s what I’ll do.”
However, if they have had a different conversation with the doctor, the same patient may conclude:
“I’ve been really worried about whether I can go through with what is going to happen from here. However, I’ve had a good discussion with the doctor. Doctor says they’ve helped lots of patients through these final stages and she and her colleagues will be with me every step of the way. She says there are very good pain relief medicines these days and they can almost always relieve pain and other symptoms. She says she has seen lots of patients use their final weeks to make their peace with the world, say their farewells to loved ones and sort out any loose ends in their life. I don’t want to die, but I’m now going to make the most of whatever time I’ve got left.”
It is of course those patients who are marginalised and disadvantaged, or who have grown up to believe that “doctor knows best”, who are most vulnerable to and dependent on the treating doctor for the advice and guidance that will determine their decision.
If assisted suicide is legalised, the systemic risks of inadequate or erroneous advice will arise in multiple ways.
Most pervasively, once Parliament has characterised the question of assisted suicide or not as simply an exercise of autonomous patient choice, doctors will be increasingly likely to respond to patients asking about assisted suicide by providing a purely factual presentation of options, rather than recognising that they also have a professional responsibility to respond to the patient’s vulnerability and need for reassurance and emotional support in order to lay unfounded fears to rest.
As well, if the UK is like Victoria, many doctors advising patients will not have good knowledge of what palliative care options are available or of what specialist palliative care can achieve, and therefore will be at risk of misadvising their patients even if they are trying to do their best. Based on the doctor’s poor advice, many of these patients may decide to accept assisted suicide, whereas otherwise they would have found out that palliative care could do more than their doctor thought, that their fears about dying in pain were unfounded and that their existential fears were able to be resolved.
Further, as in Victoria, the provision of assisted suicide is likely to be concentrated with those doctors whose personal views are inclined toward assisted suicide and whose practices have been geared to handle the procedural steps involved. Many of those doctors will in fact be strongly supportive of an assisted suicide regime, and strongly inclined to think it is the best choice for many patients. In consequence, there is a high risk of their views resulting in them not properly advising their patients about what palliative care could do or about what their likely experiences through to end of life would be, and of not being alert to risks of depression, coercion or lack of capacity.
As well as these attitude changes in medical practice, legalising assisted suicide is likely to shape the attitudes of family and friends away from fighting to get the best possible palliative care and other supports for their loved one and towards thinking that if Parliament says assisted suicide is OK, it might be the best outcome for the distress that the patient’s suffering is causing for everyone involved, thus leading them to validate the patient thinking along those lines.
No independent review, such as by the High Court, is going to be able to protect against these effects of the attitude changes that legalising assisted suicide will produce, because the misadvised patient, often validated by family and friends, will believe they are taking the best course available to them, and the misadvising doctors will be oblivious to the fact that they could and should have given the patient better advice and support.
Furthermore, while I’m not a UK legal practitioner, it seems to me that the Bill’s High Court procedures would struggle to play even the limited role the Bill’s supporters presumably claim, namely, to protect against doctors who don’t comply with the legislation and against patients being induced or browbeaten into seeking VAD by abusive or manipulative family members.
For a start, the sheer volume of cases involved seems likely to be overwhelming. A rough extrapolation of Victorian numbers would suggest 5,000 or so cases a year would come before the court. I see that Sir James Munby, the former President of the Family Division of the High Court, has put the estimate even higher, at 17,000 cases a year. On Sir James’ estimate, even if every one of the 19 Family Division judges sat full time on assisted suicide cases alone there would only be 19,000 sitting hours a year available for hearings, and even that would be impossible given the many other cases the Family Division also needs to hear.
This apparent impossibility of the High Court coping with hearings for the numbers of cases involved strongly suggests that the Bill has not been properly thought through by its proponents. Furthermore, if the Bill is predicated on such a fundamental flaw as this, how many other fundamental flaws does it have as well?
Besides this small matter of logistics, there’s the question of how a judge is supposed to properly ensure everything is in order when all the judge has to go on is the evidence largely if not wholly supplied and presented by the supporting doctor. This is particularly so given that many of the doctors involved in these cases are likely to be committed supporters of an assisted suicide regime. With no contradicting party to the proceedings, unless there is something overlooked in the evidence presented to the court that gives rise to suspicion, the court is unlikely to become aware of any contradictory evidence. Yet many of the risks which the judge most needs to guard against will consist of subtle pressure or clinically depressed patients, where careful and in-person assessment is required of how witnesses respond to questions.
A further concern is that the Bill does not provide for appeal against a judge’s decision to make a declaration authorising an assisted suicide, even if there’s an obvious error or failure, or if new evidence comes to light pointing to coercion or other factors not known at the time of the hearing.
Last but not least is the uncertainty that Sir James Munby has highlighted about whether or not under the Bill an actual hearing needs to take place at all, or whether applications will be able to be decided on the papers simply by a judge or other court officer reviewing the documentation in their chambers and only convening a hearing if there happens to be some defect or concern in the paperwork.
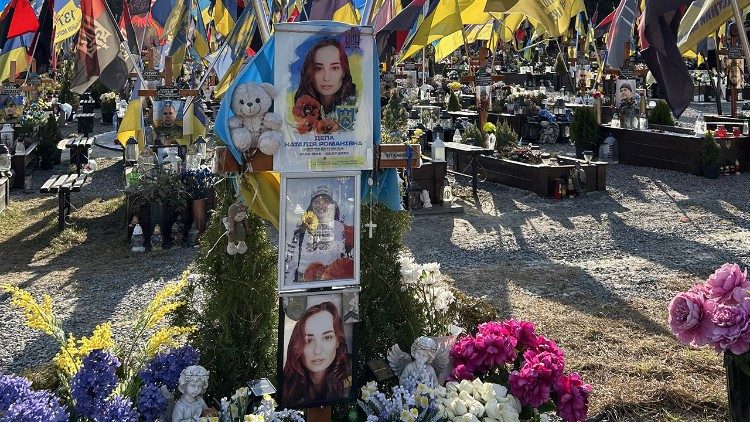
(Disability campaigners from “Distant Voices and Not Dead” hold a demonstration outside Westminster Hall in central London, on April 29, 2024, protesting against proposals to legalise assisted suicide in the UK | Photo by BEN STANSALL/AFP via Getty Images)
![]()
The post ‘Hear no evil, see no evil, speak no evil’: Former Attorney-General in Victoria, Australia, on how assisted suicide legislation really works appeared first on Catholic Herald.